Subarchnoid haemorrhage
Subarachnoid hemorrhage (SAH) is least common type of stroke

- Head trauma is the most common cause.
In patients without head trauma, SAH is most commonly caused by a brain aneurysm. A brain aneurysm is a ballooning of an artery in the brain that can rupture and bleed into the space between the brain and the skull.
- Risk factors for developing an aneurysm include:
- High blood pressure
- Smoking cigarettes
- Drug abuse like :Excessive alcohol Cocaine and/or methamphetamine use
- Family history of brain aneurysm
- Certain types of connective tissue disorders
- Prior brain aneurysm
SYMPTOMS AND CAUSES
What are the RED ALERT symptoms for subarachnoid hemorrhage (SAH)?
Most subarachnoid hemorrhages caused by a ruptured brain aneurysm is an emergency and 9-1-1 should be called immediately. Symptoms of a ruptured brain aneurysm include:
- Sudden worst headache of life (On Pain scale 10/10)
- Associated neck or back pain
- Nausea and vomiting
- Decreased responsiveness
- Sudden weakness
- Dizziness
- Seizure


DIAGNOSIS AND TESTS
How is a subarachnoid hemorrhage (SAH) diagnosed?
- Computerized tomography (CT scan) of the brain is a simple, effective way to see a subarachnoid hemorrhage.
- CT angiography (CTA) visualizes blood vessels using contrast material injected intravenously (through a vein). Sometimes, a CT scan may miss a very small subarachnoid hemorrhage, or one that has occurred a week or two ago.
- their tests may be ordered to detect a subarachnoid hemorrhage if a CT scan is negative.
These tests include:
- Lumbar puncture. A small needle is placed in the lowest part of the back to obtain cerebrospinal fluid, the fluid that bathes our brain and spinal cord. The fluid is tested for subarachnoid hemorrhage.
- Magnetic resonance imaging (MRI) of the brain. This imaging test can show if there has been “subacute” blood, or bleeding in the brain, in the recent past.


Other tests given after subarachnoid hemorrhage (SAH) is diagnosed
Aneurysm detection
Digital substraction Angiography (DSA) BRAIN And NECK
The most common test performed to best see the brain’s blood vessels is a cerebral angiogram. A catheter is placed in the main artery in the groin (femoral artery) or wrist (radial artery). Through this a thinner catheter is advanced through the body’s arterial system into the neck. Contrast material is then injected and the X-ray pictures capture the blood flowing in the brain’s arteries and brains.
Occasionally, subarachnoid hemorrhages may be caused by other brain or spine vascular lesions. An MRI of the brain and/or spine may be ordered if a cerebral angiogram does not demonstrate a brain aneurysm.
A much rarer vascular cause for subarachnoid hemorrhage, benign perimesencephalic SAH is a type of SAH in which no vascular lesion is found on imaging. Some theories regarding cause include bleeding from a vein or from a blood clot in the blood vessel wall.
MEDICAL MANAGEMENT OF SAH
MANAGEMENT AND TREATMENT
How is SAH from brain aneurysm treated?
1. Securing a brain aneurysm
There are broadly two methods : open surgery or endovascular treatment.
Endovascular treatment of an aneurysm is a minimally invasive option using cerebral angiography to access the aneurysm. The decision on which treatment is best depends on the characteristics of the aneurysm and overall health of the patient.
The surgical team will discuss these options and recommendations for which treatment is best.
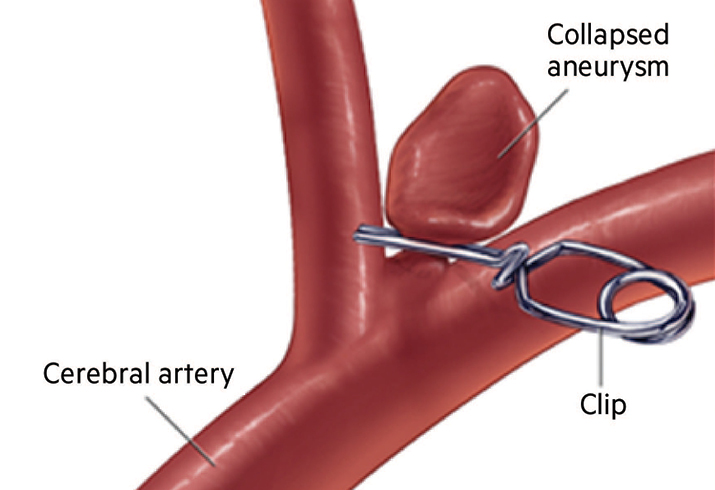
2. Open surgical techniques: clipping or bypass
Clipping. One treatment for securing a brain aneurysm is through microsurgical clipping. This surgery requires a craniotomy. A craniotomy is performed by making an incision on the head and temporarily removing a small portion of skull. After the brain is exposed, the surgical team uses an intraoperative microscope to dissect through the brain to access the aneurysm. Once the aneurysm is visualized, a small clip is placed around the base, or neck, of the aneurysm. The skull portion is replaced and fastened with plates and screws, and the incision is closed.

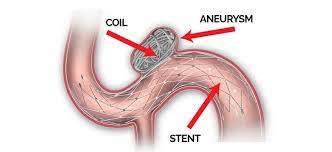
- Stenting/flow diversion. A newer device used to treat aneurysms is called a flow diversion device. These special types of stents (tubes) are placed across the base of the aneurysm and reduce blood flow into the aneurysm, causing a clot to form in the aneurysm and eventually cure it. A patient who receives a stent or flow diversion device is also prescribed medications to prevent clots from forming within the stent of the flow diversion device. Specific medications and duration of treatment may vary.
Preventing aneurysm rebleeding
Once an aneurysm has ruptured, there is an increased chance that it can rebleed. Brain aneurysm rebleeding is dangerous and can be fatal. The chance of rebleeding can be reduced by:
- Securing the aneurysm
- Controlling blood pressure
- Correcting any bleeding disorder or reversing certain types of blood thinning medications.
- Vessel bypass. If the aneurysm is a type that won’t allow straightforward microsurgical clipping, vessel bypass may be done. Endovascular surgical techniques: coiling and/or stenting/flow diversion
Endovascular treatment is a minimally invasive method to treat brain aneurysms.
- Coiling. A cerebral angiogram is performed, passing a catheter into the brain. When an aneurysm is coiled, a catheter is extended into the base of the aneurysm and platinum coils are released into the aneurysm. These coils fold in such a way as to fill the aneurysm. The coils then form a clot to prevent any further blood flow into the aneurysm. There are times when a stent may be used to support the coils remaining in the aneurysm and protect normal blood flow through the artery.
How are possible complications from subarachnoid hemorrhage from brain aneurysm treated?
Brain swelling and hydrocephalus
Complications from SAH can include brain swelling and hydrocephalus.
Bleeding from a subarachnoid hemorrhage can cause swelling of the brain, which can be life threatening.
Medications can be used to reduce brain swelling.
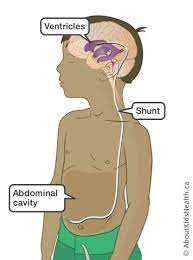
The bleeding that occurs in SAH can cause an obstruction in the ventricles that blocks the fluid from passing through and these spaces get larger. This bleeding can also interfere with the brain’s ability to reabsorb the fluid normally.
Hydrocephalus can be potentially dangerous if untreated. The treatment for hydrocephalus is to drain the excess fluid (see below).
External ventricular drain (EVD). An external ventricular drain, or EVD, is a drain placed in the ventricle of the brain to serve both as a monitor for intracranial pressure (ICP), as well as a treatment for brain swelling and hydrocephalus.

Shunt surgery. A shunt surgery permanently places a drain from the ventricles into the peritoneal cavity of the abdomen to treat hydrocephalus.
Seizures
A seizure is an over-excitability of a brain cell’s electrical discharges. A patient can have a seizure that causes shaking of one part or all of the body. Or “silent” seizures may occur, which may cause sleepiness but are not otherwise clinically detected. They may also require longer-term therapy based upon the treatment and whether or not they actually seize.
Some patients require monitoring for seizures with an electroencephalogram (EEG).
An EEG is a test that uses electrodes temporarily attached to the scalp that show abnormalities in the brain’s electrical activity.
Vasospasm and treatment methods
After an aneurysm ruptures, the brain’s arteries may begin to narrow due to the presence of the blood and inflammation. This condition is called vasospasm. If the vasospasm is significant (called clinical vasospasm), a patient may develop neurologic changes and even suffer an ischemic stroke.
The peak period for development of vasospasm occurs between the 7th and 10th days after the aneurysm bleeds, but may extend to 14 days or longer after the hemorrhage.
- Close neurologic monitoring is key in monitoring for vasospasm. Other tests such as transcranial Doppler (TCD) may be used in monitoring for vasospasm.
- The medication nimodipine is thought to improve outcomes from vasospasm following subarachnoid hemorrhage.
- Maintaining hydration is key and is monitored closely.
How long are hospital stays for subarachnoid hemorrhage (SAH)?
Length of stay in the hospital varies based on patients’ clinical status.
Most patients are admitted in the hospital anywhere from 10 to 20 days based on their condition, need for rehabilitation, and the presence and/or course of vasospasm.
Patients diagnosed with benign perimesencephalic subarachnoid hemorrhage are usually discharged within 1 week.
LIVING WITH
What follow up is needed after subarachnoid hemorrhage (SAH)?
Patients are often seen in outpatient neurosurgical follow up after 1 month with a CT brain to evaluate neurologic recovery and evaluate for delayed hydrocephalus.
Hydrocephalus can occasionally occur weeks after a hemorrhage if there is slow imbalance between the brain’s production and reabsorption of cerebrospinal fluid.
Additional follow up with aneurysm imaging depends on the aneurysm’s initial treatment and the appearance of the aneurysm at discharge.
It is important to maintain a long-term relationship with the cerebrovascular neurosurgical group for aneurysm monitoring.
What is recovery after a subarachnoid hemorrhage (SAH)?
Recovery after a subarachnoid hemorrhage widely varies based upon the cause and the extent of neurologic injury.
Most patients with subarachnoid hemorrhage from an aneurysm require inpatient rehabilitation after the hospital stay, as well as outpatient therapy for months following.
Feeling sad or anxious about the hospital stay or the illness is common. It is important to discuss these feelings with friends and family, as well as the medical team