SPINE ISSUE
NECK PAIN
Neck pain is a common complaint. Neck muscles can be strained from poor posture — whether it’s leaning over your computer or hunching over your workbench. Osteoarthritis also is a common cause of neck pain.
Rarely, neck pain can be a symptom of a more serious problem. Seek medical care if your neck pain is accompanied by numbness or loss of strength in your arms or hands or if you have shooting pain into your shoulder or down your arm.
Symptoms
- Pain that’s often worsened by holding your head in one place for long periods, such as when driving or working at a computer
- Muscle tightness and spasms
- Decreased ability to move your head
- Headache
When to see a doctor
Most neck pain improves gradually with home treatment. If not, see your doctor.
Seek immediate care if severe neck pain results from an injury, such as a motor vehicle accident, diving accident or fall.
Contact a doctor if your neck pain:
- Is severe
- Persists for several days without relief
- Spreads down arms or legs
- Is accompanied by headache, numbness, weakness or tingling
Causes
Your neck is flexible and supports the weight of your head, so it can be vulnerable to injuries and conditions that cause pain and restrict motion. Neck pain causes include:
- Muscle strains.Overuse, such as too many hours hunched over your computer or smartphone, often triggers muscle strains. Even minor things, such as reading in bed or gritting your teeth, can strain neck muscles.
- Worn joints.Just like the other joints in your body, your neck joints tend to wear down with age. Osteoarthritis causes the cushions (cartilage) between your bones (vertebrae) to deteriorate. Your body then forms bone spurs that affect joint motion and cause pain.
- Nerve compression.Herniated disks or bone spurs in the vertebrae of your neck can press on the nerves branching out from the spinal cord.
- Rear-end auto collisions often result in whiplash injury, which occurs when the head is jerked backward and then forward, straining the soft tissues of the neck.
- Certain diseases, such as rheumatoid arthritis, meningitis or cancer, can cause neck pain.
Prevention
Most neck pain is associated with poor posture combined with age-related wear and tear.
Some simple changes in your daily routine may help. Consider trying to:
- Use good posture.When standing and sitting, be sure your shoulders are in a straight line over your hips and your ears are directly over your shoulders.
- Take frequent breaks.If you travel long distances or work long hours at your computer, get up, move around and stretch your neck and shoulders.
- Adjust your desk, chair and computerso that the monitor is at eye level. Knees should be slightly lower than hips. Use your chair’s armrests.
- Avoidtucking the phone between your ear and shoulder when you talk. Use a headset or speakerphone instead.
- If you smoke, quit.Smoking can put you at higher risk of developing neck pain.
- Avoid carrying heavy bags with straps over your shoulder.The weight can strain your neck.
- Sleep in a good position.Your head and neck should be aligned with your body. Use a small pillow under your neck. Try sleeping on your back with your thighs elevated on pillows, which will flatten your spinal muscles.
Diagnosis
Your doctor will take a medical history and do an exam. He or she will check for tenderness, numbness and muscle weakness, as well as see how far you can move your head forward, backward and side to side.
Imaging tests
Your doctor might order imaging tests to get a better picture of the cause of your neck pain. Examples include:
- X-rays. X-rays can reveal areas in your neck where your nerves or spinal cord might be pinched by bone spurs or other degenerative changes.
- MRI uses radio waves and a strong magnetic field to create detailed images of bones and soft tissues, including the spinal cord and the nerves coming from the spinal cord.
- Electromyography (EMG).If your doctor suspects your neck pain might be related to a pinched nerve, he or she might suggest an EMG. It involves inserting fine needles through your skin into a muscle and performing tests to measure the speed of nerve conduction to determine whether specific nerves are functioning properly.
- Blood tests. Blood tests can sometimes provide evidence of inflammatory or infectious conditions that might be causing or contributing to your neck pain.
Treatment
The most common types of mild to moderate neck pain usually respond well to self-care within two or three weeks. If neck pain persists, your doctor might recommend other treatments.
Medications
Your doctor might prescribe stronger pain medicine than what you can get over-the-counter, as well as muscle relaxants and tricyclic antidepressants for pain relief.
Therapy
- Physical therapy.A physical therapist can teach you correct posture, alignment and neck-strengthening exercises, and can use heat, ice, electrical stimulation and other measures to help ease your pain and prevent a recurrence.
- Transcutaneous electrical nerve stimulation (TENS).Electrodes placed on your skin near the painful areas deliver tiny electrical impulses that may relieve pain.
- Traction uses weights, pulleys or an air bladder to gently stretch your neck. This therapy, under supervision of a medical professional and physical therapist, may provide relief of some neck pain, especially pain related to nerve root irritation.
- Short-term immobilization.A soft collar that supports your neck may help relieve pain by taking pressure off the structures in your neck. However, if used for more than three hours at a time or for more than one to two weeks, a collar might do more harm than good.
- Steroid injections.Your doctor might inject corticosteroid medications near the nerve roots, into the small facet joints in the bones of the cervical spine or into the muscles in your neck to help with pain. Numbing medications, such as lidocaine, also can be injected to relieve your neck pain.
- Rarely needed for neck pain, surgery might be an option for relieving nerve root or spinal cord compression.
· Lifestyle and home remedies
- Alternate heat and cold.Reduce inflammation by applying cold, such as an ice pack or ice wrapped in a towel, for up to 20 minutes several times a day. Or alternate the cold treatment with heat. Try taking a warm shower or using a heating pad on the low setting.
- Home exercises.Once the worst of your pain has subsided, begin gentle stretching exercises daily. Your doctor or a physical therapist can instruct you in the proper technique. First warm your neck and back with a heating pad or in the shower or bath. Then gently tilt, bend and rotate your neck.
Alternative medicine
Talk to your doctor if you’re interested in trying alternative treatments for your neck pain. Your doctor can discuss the benefits and risks. Alternative treatments include:
- Acupuncture involves the insertion of thin needles into various points on your body. Studies have found that acupuncture may be helpful for many types of pain. But studies in neck pain have been mixed. For best results, you may need to undergo several acupuncture sessions. Acupuncture is generally considered safe when performed by a certified practitioner using sterile needles.
- Performed mainly on the spine, a chiropractic adjustment applies a controlled, abrupt force to a joint. Chiropractic treatments to the neck can provide short-term pain relief, and, for many people, carry minimal risks.
- During a massage, a trained practitioner manipulates the muscles in your neck with his or her hands. Little scientific evidence exists to support massage in people with neck pain, though it may provide relief when combined with your doctor’s recommended treatments.
Preparing for your appointment
You might initially contact your family doctor about your neck pain, and he or she may refer you to:
- A doctor who specializes in nonoperative treatment of musculoskeletal conditions (physical medicine and rehabilitation)
- A doctor who specializes in arthritis and other diseases that affect the joints (rheumatologist)
- A doctor who specializes in treating nerve-related disorders (neurologist)
- A doctor who operates on bones and joints (orthopedic surgeon)
What you can do
Before your appointment, you may want to write a list of answers to the following questions:
- When did your symptoms begin?
- Have you ever injured your neck? If so, when did the injury occur?
- Do any particular neck movements improve or worsen the pain?
- What medications and supplements do you take regularly?
What to expect from your doctor
Your doctor might ask some of the following questions:
- Where exactly does your pain occur?
- Is the pain dull, sharp or shooting?
- Do you have numbness or weakness?
- Does the pain radiate into your arm?
- Is the pain made worse by straining, coughing or sneezing?
- Do you have other physical problems?
LOW BACK PAIN

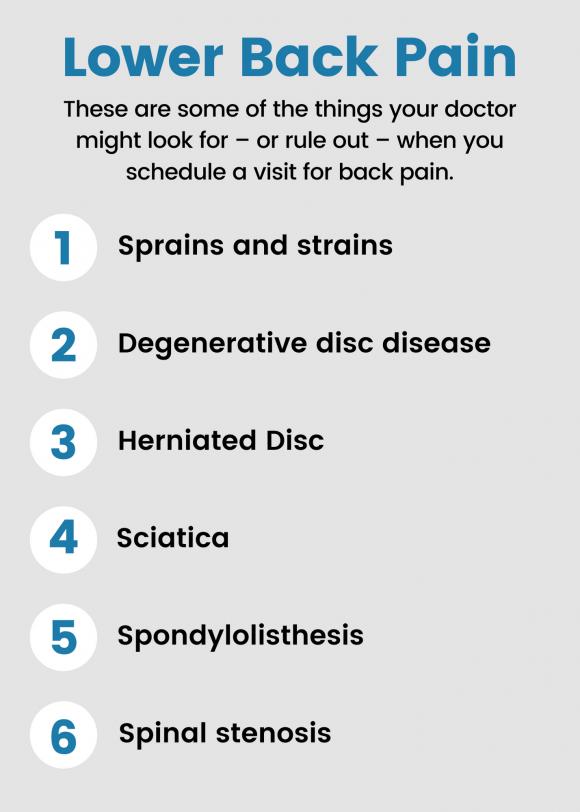
A common, painful condition affecting the lower portion of the spine.
Low back pain is caused by injury to a muscle (strain) or ligament (sprain).
Common causes include improper lifting, poor posture, lack of regular exercise, a fracture, a ruptured disc or arthritis. Often, the only symptom is pain in the lower back.
When to see a doctor
Most back pain gradually improves with home treatment and self-care, usually within a few weeks. Contact your doctor if your back pain:
- Persists for past a few weeks
- Is severe and doesn’t improve with rest
- Spreads down one or both legs, especially if the pain extends below the knee
- Causes weakness, numbness or tingling in one or both legs
- Is accompanied by unexplained weight loss
In rare cases, back pain can signal a serious medical problem. Seek immediate care if your back pain:
- Causes new bowel or bladder problems
- Is accompanied by a fever
- Follows a fall, blow to your back or other injury.
CAUSES
Back pain often develops without a cause that your doctor can identify with a test or an imaging study. Conditions commonly linked to back pain include:
- Muscle or ligament strain. Repeated heavy lifting or a sudden awkward movement can strain back muscles and spinal ligaments. If you’re in poor physical condition, constant strain on your back can cause painful muscle spasms.
- Bulging or ruptured disks. Disks act as cushions between the bones (vertebrae) in your spine. The soft material inside a disk can bulge or rupture and press on a nerve. However, you can have a bulging or ruptured disk without back pain. Disk disease is often found incidentally when you have spine X-rays for some other reason.
- Osteoarthritis can affect the lower back. In some cases, arthritis in the spine can lead to a narrowing of the space around the spinal cord, a condition called spinal stenosis.
- Your spine’s vertebrae can develop painful fractures if your bones become porous and brittle.
Risk factors
- Back pain is more common as you get older, starting around age 30 or 40.
- Lack of exercise. Weak, unused muscles in your back and abdomen might lead to back pain.
- Excess weight. Excess body weight puts extra stress on your back.
- Some types of arthritis and cancer can contribute to back pain.
- Improper lifting. Using your back instead of your legs can lead to back pain.
- Psychological conditions. People prone to depression and anxiety appear to have a greater risk of back pain.
- Smokers have increased rates of back pain. This may occur because smoking prompts more coughing, which can lead to herniated disks. Smoking can also decrease blood flow to the spine and increase the risk of osteoporosis.
Prevention
You might avoid back pain or prevent its recurrence by improving your physical condition and learning and practicing proper body mechanics.
- Regular low-impact aerobic activities — those that don’t strain or jolt your back — can increase strength and endurance in your back and allow your muscles to function better. Walking and swimming are good choices. Talk with your doctor about which activities you might try.
- Build muscle strength and flexibility. Abdominal and back muscle exercises, which strengthen your core, help condition these muscles so that they work together like a natural corset for your back.
- Maintain a healthy weight. Being overweight strains back muscles. If you’re overweight, trimming down can prevent back pain.
- Quit smoking. Smoking increases your risk of low back pain. The risk increases with the number of cigarettes smoked per day, so quitting should help reduce this risk.
Avoid movements that twist or strain your back. Use your body properly:
- Stand smart. Don’t slouch. Maintain a neutral pelvic position. If you must stand for long periods, place one foot on a low footstool to take some of the load off your lower back. Alternate feet. Good posture can reduce the stress on back muscles.
- Sit smart. Choose a seat with good lower back support, armrests and a swivel base. Placing a pillow or rolled towel in the small of your back can maintain its normal curve. Keep your knees and hips level. Change your position frequently, at least every half-hour.
- Lift smart. Avoid heavy lifting, if possible, but if you must lift something heavy, let your legs do the work. Keep your back straight — no twisting — and bend only at the knees. Hold the load close to your body. Find a lifting partner if the object is heavy or awkward.
Buyer beware
Because back pain is so common, numerous products promise prevention or relief. But there’s no definitive evidence that special shoes, shoe inserts, back supports, specially designed furniture or stress management programs can help.
In addition, there doesn’t appear to be one type of mattress that’s best for people with back pain. It’s probably a matter of what feels most comfortable to you.
SPINAL CORD TRAUMA
Emergency signs and symptoms:
- Extreme back pain or pressure in your neck, head or back
- Weakness, incoordination or paralysis in any part of your body
- Numbness, tingling or loss of sensation in your hands, fingers, feet or toes
- Loss of bladder or bowel control
- Difficulty with balance and walking
- Impaired breathing after injury
- An oddly positioned or twisted neck or back
When to see a doctor
Anyone who experiences significant trauma to his or her head or neck needs immediate medical evaluation for the possibility of a spinal injury. In fact, it’s safest to assume that trauma victims have a spinal injury until proved otherwise because:
- A serious spinal injury isn’t always immediately obvious. If it isn’t recognized, a more severe injury may occur.
- Numbness or paralysis may occur immediately or come on gradually as bleeding or swelling occurs in or around the spinal cord.
- The time between injury and treatment can be critical in determining the extent and severity of complications and the possible extent of expected recovery.
If you suspect that someone has a back or neck injury:
- Don’t move the injured person — permanent paralysis and other serious complications may result
- Cal local emergency medical assistance number
- Keep the person still.
- Place heavy towels on both sides of the neck or hold the head and neck to prevent them from moving until emergency care arrives
- Provide basic first aid, such as stopping any bleeding and making the person comfortable, without moving the head or neck.
Common causes of spinal cord injuries:
- Motor vehicle accidents. Auto and motorcycle accidents are the leading cause of spinal cord injuries, accounting for almost half of new spinal cord injuries each year.
- Falls. A spinal cord injury after age 65 is most often caused by a fall. Overall, falls cause about 31% of spinal cord injuries.
- Acts of violence. Over 13% of spinal cord injuries result from violent encounters, most commonly involving gunshot wounds. Knife wounds also are common.
- Sports and recreation injuries. Athletic activities, such as impact sports and diving in shallow water, cause about 10% of spinal cord injuries.
- Alcohol. Alcohol use is a factor in about 1 out of every 4 spinal cord injuries.
- Diseases. Cancer, arthritis, osteoporosis and inflammation of the spinal cord also can cause spinal cord injuries.
Risk factors
- Being male. Spinal cord injuries affect a disproportionate number of men. In fact, females account for only about 20% of traumatic spinal cord injuries in the United States.
- Being between the ages of 16 and 30.You’re most likely to suffer a traumatic spinal cord injury if you’re between the ages of 16 and 30. The average age at time of injury is 43 years.
- Being older than 65.Falls cause most injuries in older adults.
- Engaging in risky behavior. Diving into too-shallow water or playing sports without wearing the proper safety gear or taking proper precautions can lead to spinal cord injuries. Motor vehicle crashes are the leading cause of spinal cord injuries for people under 65.
- Having a bone or joint disorder. A relatively minor injury can cause a spinal cord injury if you have another disorder that affects your bones or joints, such as arthritis or osteoporosis.
Complications
- Bladder control. Your bladder will continue to store urine from your kidneys. However, your brain may not be able to control your bladder as well because the message carrier (the spinal cord) has been injured.
The changes in bladder control increase your risk of urinary tract infections. The changes may also cause kidney infections and kidney or bladder stones. During rehabilitation, you’ll learn new techniques to help empty your bladder.
- Bowel control. Although your stomach and intestines work much like they did before your injury, control of your bowel movements is often altered. A high-fiber diet may help regulate your bowels, and you’ll learn techniques to optimize your bowel function during rehabilitation.
- Skin sensation. Below the neurological level of your injury, you may have lost part of or all skin sensations. Therefore, your skin can’t send a message to your brain when it’s injured by certain things such as prolonged pressure, heat or cold.
This can make you more susceptible to pressure sores, but changing positions frequently — with help, if needed — can help prevent these sores. You’ll learn proper skin care during rehabilitation, which can help you avoid these problems.
- Circulatory control. A spinal cord injury may cause circulatory problems ranging from low blood pressure when you rise (orthostatic hypotension) to swelling of your extremities. These circulation changes may also increase your risk of developing blood clots, such as deep vein thrombosis or a pulmonary embolus.
Another problem with circulatory control is a potentially life-threatening rise in blood pressure (autonomic hyperreflexia). Your rehabilitation team will teach you how to address these problems if they affect you.
- Respiratory system. Your injury may make it more difficult to breathe and cough if your abdominal and chest muscles are affected. These include the diaphragm and the muscles in your chest wall and abdomen.
Your neurological level of injury will determine what kind of breathing problems you may have. If you have a cervical and thoracic spinal cord injury, you may have an increased risk of pneumonia or other lung problems. Medications and therapy can help prevent and treat these problems.
- Muscle tone. Some people with spinal cord injuries experience one of two types of muscle tone problems: uncontrolled tightening or motion in the muscles (spasticity) or soft and limp muscles lacking muscle tone (flaccidity).
- Fitness and wellness. Weight loss and muscle atrophy are common soon after a spinal cord injury. Limited mobility may lead to a more sedentary lifestyle, placing you at risk of obesity, cardiovascular disease and diabetes.
A dietitian can help you eat a nutritious diet to sustain an adequate weight. Physical and occupational therapists can help you develop a fitness and exercise program.
- Sexual health. Sexuality, fertility and sexual function may be affected by a spinal cord injury. Men may notice changes in erection and ejaculation; women may notice changes in lubrication. Physicians specializing in urology or fertility can offer options for sexual functioning and fertility.
- Some people experience pain, such as muscle or joint pain, from overuse of particular muscle groups. Nerve pain can occur after a spinal cord injury, especially in someone with an incomplete injury.
- Coping with all the changes a spinal cord injury brings and living with pain causes some people to experience depression.
Prevention
Following this advice may reduce your risk of a spinal cord injury:
- Drive safely. Car crashes are one of the most common causes of spinal cord injuries. Wear a seat belt every time you drive or ride in a car.
Make sure that your children wear a seat belt or use an age- and weight-appropriate child safety seat. To protect them from air bag injuries, children under age 12 should always ride in the back seat.
- Check water depth before diving. To make sure you don’t dive into shallow water, don’t dive into a pool unless it’s 12 feet (about 3.7 meters) or deeper, don’t dive into an aboveground pool, and don’t dive into any water of which you don’t know the depth.
- Prevent falls. Use a step stool with a grab bar to reach objects in high places. Add handrails along stairways. Put nonslip mats on tile floors and in the tub or shower. For young children, use safety gates to block stairs and consider installing window guards.
- Take precautions when playing sports. Always wear recommended safety gear. Avoid leading with your head in sports. For example, don’t slide headfirst in baseball, and don’t tackle using the top of your helmet in football. Use a spotter for new moves in gymnastics.
- Don’t drink and drive. Don’t drive while intoxicated or under the influence of drugs. Don’t ride with a driver who’s been drinking.
DIAGNOSIS
- X-rays. Medical personnel typically order these tests on people who are suspected of having a spinal cord injury after trauma. X-rays can reveal vertebral (spinal column) problems, tumors, fractures or degenerative changes in the spine.
- Computerized tomography (CT) scan. A CT scan may provide a better look at abnormalities seen on an X-ray. This scan uses computers to form a series of cross-sectional images that can define bone, disk and other problems.
- Magnetic resonance imaging (MRI). MRI uses a strong magnetic field and radio waves to produce computer-generated images. This test is very helpful for looking at the spinal cord and identifying herniated disks, blood clots or other masses that may be compressing the spinal cord.
Early (acute) stages of treatment
- Maintaining your ability to breathe
- Preventing shock
- Immobilizing your neck to prevent further spinal cord damage
Avoiding possible complications, such as stool or urine retention, respiratory or cardiovascular difficulty, and formation of deep vein blood clots in the extremities.
Medications.
Intravenous (IV) methylprednisolone has been used as a treatment option for an acute spinal cord injury in the past. But recent research has shown that the potential side effects, such as blood clots and pneumonia, from using this medication outweigh the benefits. Because of this, methylprednisolone is no longer recommended for routine use after a spinal cord injury.
- Immobilization. You may need traction to stabilize your spine, to bring the spine into proper alignment or both. In some cases, a rigid neck collar may work. A special bed also may help immobilize your body.
- Surgery. Often surgery is necessary to remove fragments of bones, foreign objects, herniated disks or fractured vertebrae that appear to be compressing the spine. Surgery may also be needed to stabilize the spine to prevent future pain or deformity.
- Experimental treatments. Scientists are trying to figure out ways to stop cell death, control inflammation and promote nerve regeneration. For example, doctors may lower the body temperature significantly — a condition known as hypothermia — for 24 to 48 hours to help prevent damaging inflammation. Ask your doctor about the availability of such treatments.
Prognosis and recovery
Your doctor may not be able to give you a prognosis right away. Recovery, if it occurs, typically starts a week to six months after an injury. The fastest rate of recovery is often seen in the first six months, but some people experience small improvements for up to one to two years.