NERVE DISEASE
Introduction:
Peripheral nerves are thin structures located in your arms, legs, and throughout your body. When one or more of these nerves become damaged—as a result of an underlying disease process, medication, or infection, to name a few possibilities—a condition called peripheral neuropathy develops. The diagnosis of peripheral neuropathy requires a careful and thorough medical history and neurological examination.
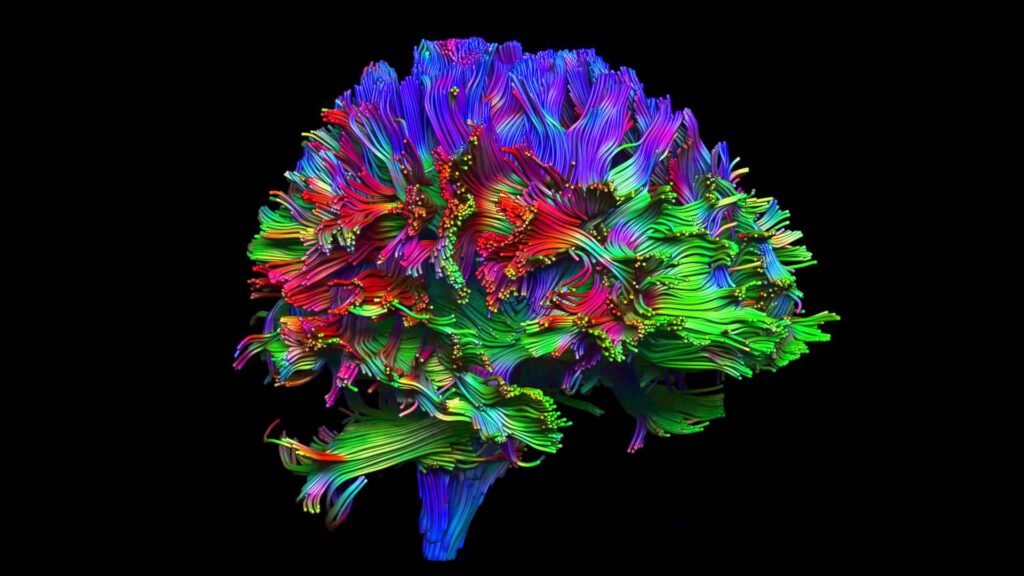
Your nervous system is divided into two parts—your central nervous system and your peripheral nervous system.
Your central nervous system consists of your brain and spinal cord. Your peripheral nervous system consists of all the nerves that are located outside of your brain and spinal cord. The function of peripheral nerves is to relay messages from your brain and spinal cord to the rest of your body, such as your arms, hands, legs, feet, internal organs, skin, and joints.
Since the peripheral nerves are not protected by the skull (as the brain is) or the vertebral spinal canal (as the spinal cord is), they are vulnerable to damage. When this happens to one or more peripheral nerves, peripheral neuropathy develops.
Types of Peripheral Neuropathy
Most of the time when you hear the term peripheral neuropathy, it’s in reference to a polyneuropathy—one of many conditions in which multiple peripheral nerves are damaged. There are also localized types of peripheral neuropathies, called mononeuropathies.
Polyneuropathy
The nerves affected by polyneuropathy may include one or more of the following:
- Sensory nerves: These nerves receive input from various locations of the body. They then send messages to the brain about the body’s sensations, such as hot and cold, pain, and touch.
- Motor nerves: These nerves transmit messages from the brain and spinal cord, telling various muscles to move.
- Autonomic nerves: These nerves regulate how your internal organs, such as your blood vessels, stomach, heart, and sweat glands, function.
Polyneuropathies are further classified based on their underlying cause.
For example, diabetic polyneuropathy is one of the most common types of polyneuropathies. It occurs as a result of nerve damage from high blood sugar levels.
While diabetic polyneuropathy predominantly affects sensory nerves, it can affect motor and autonomic nerves. Depending on what nerves are damaged, symptoms like numbness, tingling, pain, weakness, or digestive or urinary system problems may develop.
Another example of a polyneuropathy is vitamin B12 deficiency neuropathy. This disorder is more common in the elderly because they are more at risk for gut malabsorption issues.
Since vitamin B12 deficiency neuropathy affects both sensory and motor peripheral nerves, symptoms may include pain, balance problems, numbness and tingling in the hands and feet, and weakness.
A severe but uncommon type of polyneuropathy is Guillan Barré syndrome, also called acute demyelinating polyneuropathy. This dangerous disease affects both sensory and motor nerve cells and is characterized by a quickly progressive tingling and weakness, usually beginning in the feet with rapidly ascending weakness of the legs. Eventually, weakness of the muscles that control breathing occurs.
Mononeuropathy
Mononeuropathy means that a single peripheral nerve is damaged, usually as a result of trauma, compression, or entrapment.
The most classic example of a mononeuropathy is carpal tunnel syndrome, which refers to compression of the median nerve. This causes numbness and tingling in the thumb, index finger, middle finger, and part of the ring finger. If left untreated or in severe cases, hand weakness and clumsiness may develop.
Mononeuritis Multiplex
Sometimes, two or more nerves in different areas are affected. When this happens, the condition is called mononeuritis multiplex.
Blood vessel problems (for example, from an inflammatory condition called vasculitis) are typical culprits of mononeuritis multiplex.
With vasculitis neuropathy, impaired blood flow to at least two peripheral nerves results in asymmetrical pain, muscle weakness, and/or sensory disturbances.
Peripheral Neuropathy Symptoms
sensory (most common), motor, autonomic, or some combination.
Sensory
When sensory nerves are damaged, one or more of the following symptoms or signs may occur:
- Lack of sensation to pain changes in temperature
- Unusual sensations like vibration, numbness and tingling, burning, stabbing, electrical, or crawling
- Pain from a light touch that is normally painless (allodynia)
- Loss of position sense and balance problems
- Change in temperature
Motor
When motor nerves are damaged, the most common symptom is muscle weakness.
Other symptoms and signs may include:
- Muscle cramping and shrinking
- Fasciculations (when a muscle twitches without your control)
- Reflex abnormalities
Autonomic
Common symptoms and signs of autonomic nerve damage include:
- Excess sweating
- Dry skin and body hair loss
- Diarrhea
- Rapid heartbeat
- Bladder problems
- Heat intolerance
- Early satiety
- Impotence
- Orthostatic hypotension
Causes
Anything that damages one or more peripheral nerves may result in peripheral neuropathy.
- Diabetes
- Trauma or compression
- Shingles
- Alcohol abuse
- Vitamin B12 deficiency
- Hypothyroidism (an underactive thyroid gland)
- Medications – chemotherapies, are also potential culprits of peripheral neuropathy, as is heavy metal exposure, HIV infection, kidney failure, chronic liver disease, rarely, inherited diseases like Charcot-Marie-Tooth disease.
Diagnosis
The diagnosis of peripheral neuropathy begins with a neurological examination. Testing then follows, some of which will depend on what diagnoses your healthcare provider suspects based on your symptoms and medical history.
Neurological Examination
During the exam, your healthcare provider will check your reflexes and evaluate for various sensation disturbances (vibration, temperature, and pinprick), especially on your feet and hands. Your healthcare provider will also evaluate your muscle strength and your gait.
Blood Tests
In order to sort out the root cause of your peripheral neuropathy, your healthcare provider will order a series of blood tests, with some of the most common ones being:
- Complete blood count (CBC)
- Comprehensive metabolic panel (CMP)
- Erythrocyte sedimentation rate (ESR)
- Fasting blood glucose
- Vitamin B12 level
- Thyroid-stimulating hormone
Additional blood tests—for example, genetic testing for Charcot-Marie-Tooth disease or an HIV antibody test for HIV infection—may also be ordered based on your healthcare provider’s underlying suspicion.
Nerve-Specific Tests
In some cases, a nerve conduction velocity study (NCV) and electromyography (EMG) are used to confirm a diagnosis of peripheral neuropathy.
Likewise, sometimes a nerve biopsy (when a sample of nerve tissue is removed and examined under a microscope) or a neurodiagnostic skin biopsy (when a tiny piece of skin containing nerve fiber endings is removed and examined under a microscope) may be performed.
Autonomic Tests
For peripheral neuropathies with autonomic symptoms, various autonomic tests may be helpful in the diagnostic process, such as measuring a person’s heart rate response to tilt (to check for orthostatic hypotension) or tests of sweat function.
Other Tests
Besides various blood and nerve-related tests, sometimes other tests are needed to help confirm the cause of a person’s peripheral neuropathy.
For instance, a cerebrospinal fluid analysis via a lumbar puncture (spinal tap) may be performed to support a diagnose of Guillain-Barré syndrome. A 24-hour urine collection may be ordered for possible heavy metal exposure.
Differential Diagnoses
It’s important to note that during the diagnostic process for peripheral neuropathy, your healthcare provider will want to ensure that your symptoms are not due to a condition of the central nervous system (CNS), which is comprised of your brain and spinal cord.
CNS conditions that may mimic various peripheral neuropathies include stroke and multiple sclerosis (MS).
The good news is that a careful medical history and neurological exam can usually distinguish central from peripheral nervous system conditions. For example, brisk reflexes and spastic (tight, stiff) muscles may be seen with a central nervous system disease, like MS, but not with peripheral neuropathy.
Likewise, with a stroke—which is caused by inadequate blood flow in the brain—symptoms usually occur suddenly, as opposed to the symptoms of peripheral neuropathy, which develop over a longer period of time.
Treatment
Tackling the “why” behind your peripheral neuropathy is a critical first step in treatment.
if neuropathy is occurring as a result of diabetes, then obtaining better and tight control of glucose (sugar) levels may help preserve nerve function.
Likewise, if a nutritional deficiency is the neuropathy culprit, correcting it should help the neuropathy.
For medication or toxin-induced neuropathies, removing the offending agent or lowering/altering the dose may be recommended.
For other types of neuropathy, more urgent, invasive treatments are required.
For example, with Guillain-Barré syndrome, people usually require hospitalization and treatment with intravenous immunoglobulin or plasmapheresis in order to improve symptoms and shorten the disease course.