MUSCLE DISEASE
What are muscle cramps?
Muscle cramps are sudden, involuntary contractions or spasms in one or more of your muscles. They are very common and often occur after exercise. Some people get muscle cramps, especially leg cramps, at night. They can be painful, and they may last a few seconds to several minutes.
You can have a cramp in any muscle, but they happen most often in the
- Thighs
- Feet
- Hands
- Arms
- Abdomen
- Area along your ribcage
What causes muscle cramps
What causes muscle cramps?
Causes of muscle cramps include:
- Straining or overusing a muscle. This is the most common cause.
- Compression of your nerves, from problems such as a spinal cord injuryor a pinched nerve in the neck or back
- Dehydration
- Low levels of electrolytes such as magnesium, potassium, or calcium
- Not enough blood getting to your muscles
- Pregnancy
- Certain medicines
- Getting dialysis
Sometimes the cause of muscle cramps is unknown.
Who is at risk for muscle cramps?
Anyone can get muscle cramps, but they are more common in some people:
- Older adults
- People who are overweight
- Athletes
- Pregnant women
- People with certain medical conditions, such as thyroidand nerve disorders
When do I need to see a health care provider for muscle cramps?
Muscle cramps are usually harmless, and they go away after a few minutes. But you should contact your health care provider if the cramps
- Are severe
- Happen frequently
- Don’t get better with stretching and drinking enough fluids
- Last a long time
- Are accompanied by swelling, redness, or a feeling of warmth
- Are accompanied by muscle weakness
What are the treatments for muscle cramps?
You usually don’t need treatment for muscle cramps. You may be able to find some relief from cramps by
- Stretching or gently massaging the muscle
- Applying heat when the muscle is tight and ice when the muscle is sore
- Getting more fluids if you are dehydrated
If another medical problem is causing the cramps, treating that problem will likely help. There are medicines that providers sometimes prescribe to prevent cramps, but they are not always effective and may cause side effects. Talk to your provider about the risks and benefits of medicines.
Can muscle cramps be prevented?
To prevent muscle cramps, you can
- Stretch your muscles, especially before exercising. If you often get leg cramps at night, stretch your leg muscles before bed.
- Drink plenty of liquids. If you do intense exercise or exercise in the heat, sports drinks can help you replace electrolytes.
- Investigation :
- Creatine Kinase
- Electromyography (EMG) and Nerve Conduction Studies
- MRI of the Musculoskeletal System
- Needle Biopsy
FOOT DROP
Foot drop describes the inability to raise the front part of the foot due to weakness or paralysis of the muscles that lift the foot. As a result, individuals with foot drop scuff their toes along the ground or bend their knees to lift their foot higher than usual to avoid the scuffing, which causes what is called a “steppage” gait. Foot drop can be unilateral (affecting one foot) or bilateral (affecting both feet). Foot drop is a symptom of an underlying problem and is either temporary or permanent, depending on the cause. Causes include: neurodegenerative disorders of the brain that cause muscular problems, such as multiple sclerosis, stroke, and cerebral palsy; motor neuron disorders such as polio, some forms of spinal muscular atrophy and amyotrophic lateral sclerosis (commonly known as Lou Gehrig’s disease); injury to the nerve roots, such as in spinal stenosis; peripheral nerve disorders such as Charcot-Marie-Tooth disease or acquired peripheral neuropathy; local compression or damage to the
peroneal nerve as it passes across the fibular bone below the knee; and muscle disorders, such as muscular dystrophy or myositis.
Treatment depends on the specific cause of foot drop. The most common treatment is to support the foot with light-weight leg braces and shoe inserts, called ankle-foot orthotics. Exercise therapy to strengthen the muscles and maintain joint motion also helps to improve gait. Devices that electrically stimulate the peroneal nerve during footfall are appropriate for a small number of individuals with foot drop. In cases with permanent loss of movement, surgery that fuses the foot and ankle joint or that transfers tendons from stronger leg muscles is occasionally performed.
Tendonitis
Tendons are flexible bands of tissue that connect muscles to bones. They help your muscles move your bones. Tendinitis is the severe swelling of a tendon.
Tendinitis usually happens after repeated injury to an area such as the wrist or ankle. It causes pain and soreness around a joint. Some common forms of tendinitis are named after the sports that increase their risk. They include tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee.
Doctors diagnose tendinitis with your medical history, a physical exam, and imaging tests. The first step in treatment is to reduce pain and swelling. Rest, wrapping or elevating the affected area, and medicines can help. Ice is helpful for recent, severe injuries. Other treatments include ultrasound, physical therapy, steroid injections, and surgery.
Investigation
MRI of the Musculoskeletal System
Musculoskeletal Ultrasound
NEUROMUSCULAR DISORDER
Neuromuscular disorders affect your neuromuscular system.
They can cause problems with Communication between your nerves and muscles.
These disorders can cause your muscles to become weak and waste away. You may also have symptoms such as spasms, twitching, and pain.
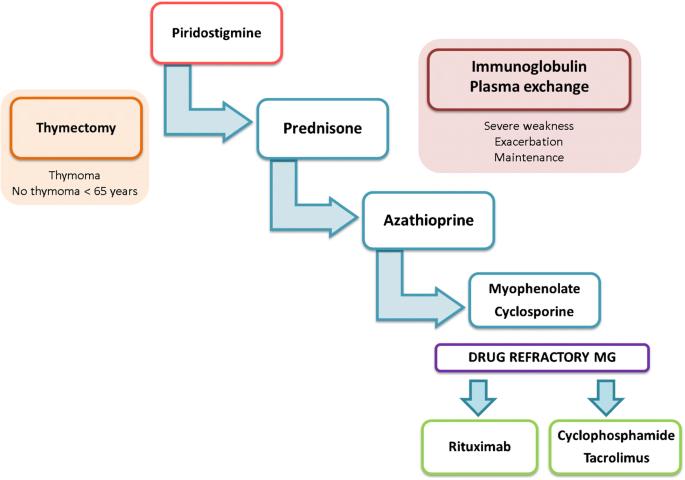
Examples of neuromuscular disorders include Myasthenia gravis

Myasthenia gravis is the prototype neuromuscular disease with immunological pathogenesis. The recognition and interpretation of the symptoms should be stressed as the diagnosis is initially achieved on clinical ground. Tests in the areas of immunology, electrophysiology and imaging further help the diagnosis, management and prognosis of the condition.
There can be different causes for these diseases. Many of them are genetic. This means they are inherited (run in families) or are caused by a new mutation in your genes. Some neuromuscular disorders are autoimmune diseases. Sometimes the cause is unknown. Many neuromuscular diseases have no cure. But treatments may improve symptoms, increase mobility, and lengthen life.
Diagnosis : Nerve Conduction studies (NCS) with Repetitive nerve stimulation (RNS) study and Electromyography (EMG)
TREATMENT:

Osteomalacic Myopathy:

Vitamin D deficiency is an important treatable cause of osteomalacic myopathy in Saudi Arabia. The diagnosis is frequently delayed or missed. Screening for Vitamin D deficiency in patients with acquired myopathy is needed to identify this treatable disorder
Muscular dystrophy

Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. In muscular dystrophy, abnormal genes (mutations) interfere with the production of proteins needed to form healthy muscle.
There are many kinds of muscular dystrophy. Symptoms of the most common variety begin in childhood, mostly in boys. Other types don’t surface until adulthood.
Causes
Certain genes are involved in making proteins that protect muscle fibers. Muscular dystrophy occurs when one of these genes is defectiveRisk factors
Muscular dystrophy occurs in both sexes and in all ages and races. However, the most common variety, Duchenne, usually occurs in young boys. People with a family history of muscular dystrophy are at higher risk of developing the disease or passing it on to their children.Associated TEST FOR DIAGNOSIS :
- Enzyme tests.Damaged muscles release enzymes, such as creatine kinase (CK), into your blood. In a person who hasn’t had a traumatic injury, high blood levels of CK suggest a muscle disease.
- Genetic testing.Blood samples can be examined for mutations in some of the genes that cause types of muscular dystrophy.
- Muscle biopsy.A small piece of muscle can be removed through an incision or with a hollow needle. Analysis of the tissue sample can distinguish muscular dystrophies from other muscle diseases.
- Heart-monitoring tests (electrocardiography and echocardiogram).These tests are used to check heart function, especially in people diagnosed with myotonic muscular dystrophy.
- Lung-monitoring tests. These tests are used to check lung function.
TREATMENT
There’s no cure for muscular dystrophy. But medications and therapy can help manage symptoms and slow the course of the disease.Complications
The complications of progressive muscle weakness include:- Trouble walking. Some people with muscular dystrophy eventually need to use a wheelchair.
- Trouble using arms. Daily activities can become more difficult if the muscles of the arms and shoulders are affected.
- Shortening of muscles or tendons around joints (contractures).Contractures can further limit mobility.
- Breathing problems. Progressive weakness can affect the muscles associated with breathing. People with muscular dystrophy might eventually need to use a breathing assistance device (ventilator), initially at night but possibly also during the day.
- Curved spine (scoliosis).Weakened muscles might be unable to hold the spine straight.
- Heart problems. Muscular dystrophy can reduce the efficiency of the heart muscle.
- Swallowing problems. If the muscles involved with swallowing are affected, nutritional problems and aspiration pneumonia can develop. Feeding tubes might be an option.
- Range-of-motion and stretching exercises. Muscular dystrophy can restrict the flexibility and mobility of joints. Limbs often draw inward and become fixed in that position. Range-of-motion exercises can help to keep joints as flexible as possible.
- Low-impact aerobic exercise, such as walking and swimming, can help maintain strength, mobility and general health. Some types of strengthening exercises also might be helpful. But it’s important to talk to your doctor first because some types of exercise might be harmful.
- Braces can help keep muscles and tendons stretched and flexible, slowing the progression of contractures. Braces can also aid mobility and function by providing support for weakened muscles.
- Mobility aids.Canes, walkers and wheelchairs can help maintain mobility and independence.
- Breathing assistance. As respiratory muscles weaken, a sleep apnea device might help improve oxygen delivery during the night. Some people with severe muscular dystrophy need to use a machine that forces air in and out of their lungs (ventilator).
What causes SMA?
Chromosome 5 SMA is caused by a deficiency of a motor neuron protein called SMN, for “survival of motor neuron.” This protein, as its name implies, seems to be necessary for normal motor neuron function. SMN plays a pivotal role in gene expression in motor neurons. Its deficiency is caused by genetic flaws (mutations) on chromosome 5 in a gene called SMN1. The most common mutation in the SMN1 gene within patients diagnosed with SMA is a deletion of a whole segment, called exon 7. What are the symptoms of SMA? SMA symptoms cover a broad spectrum, ranging from mild to severe.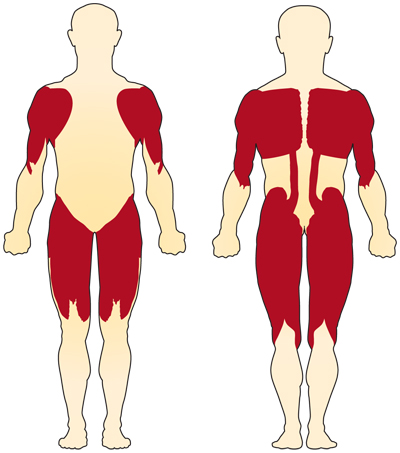
The muscles closer to the center of the body (proximal muscles) are usually more affected in SMA than are the muscles farther from the center (distal muscles).
The primary symptom of chromosome 5-related (SMN-related) SMA is weakness of the voluntary muscles. The muscles most affected are those closest to the center of the body, such as those of the shoulders, hips, thighs, and upper back. The lower limbs seem to be affected more than the upper limbs, and deep tendon reflexes are decreased.
Special complications occur if the muscles used for breathing and swallowing are affected, resulting in abnormalities in these functions. If the muscles of the back weaken, spinal curvatures can develop.
There’s a great deal of variation in the age of onset and level of motor function achieved in chromosome 5-related SMA. These are roughly correlated with how much functional SMN protein is present in the motor neurons, which in turn correlates with how many copies of SMN2 genes a person has. Sensory, mental, and emotional functioning are entirely normal in chromosome-5 SMA
TREATMENT:
It was not curable disease. Recent research showed improvement with some drugs.
On Dec. 23, 2016, the U.S. Food and Drug Administration (FDA) approved Spinraza (nusinersen) for the treatment of SMA. Spinraza is designed to treat the underlying defect in SMA, which means it potentially may be effective at slowing, stopping, or perhaps reversing the symptoms of SMA. For more, see Spinraza is Approved.
In May 2019, the FDA approved Zolgensma (onasemnogene abeparvovac-xioi), the first gene-replacement therapy for a neuromuscular disease. Zolgensma is a one-time intravenous (into the vein) infusion for the treatment of pediatric patients younger than 2 years of age with SMA with bi-allelic mutations in the SMN1 gene, including those who are presymptomatic at diagnosis.