ISCHEMIC STROKE
What is ISCHEMIC STROKE
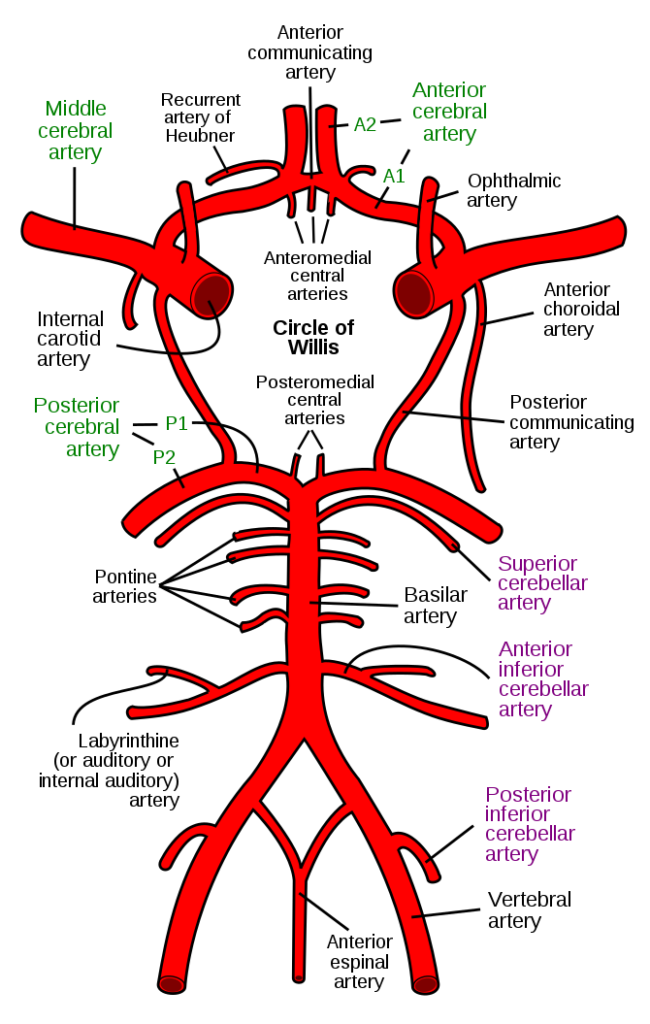
- when a blood clot blocks or narrows an artery leading to the brain.
- it accounts for about 87% of all stroke
If you or someone you’re with may be having a stroke, pay particular attention to the time the symptoms began. Some treatment options are most effective when given soon after a stroke begins.
Signs and symptoms of stroke include
- Trouble speaking and understanding what others are saying. You may experience confusion, slur your words or have difficulty understanding speech.
- Paralysis or numbness of the face, arm or leg. You may develop sudden numbness, weakness or paralysis in your face, arm or leg. This often affects just one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Also, one side of your mouth may droop when you try to smile.
- Problems seeing in one or both eyes. You may suddenly have blurred or blackened vision in one or both eyes, or you may see double.
- A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate that you’re having a stroke.
- Trouble walking. You may stumble or lose your balance. You may also have sudden dizziness or a loss of coordination.
Diagnosis of ischemic stroke
When you first arrive at hospital with a suspected stroke, the doctor will want to find out as much as they can about your symptoms.
A number of tests can be done to confirm the diagnosis and determine the cause of the stroke.
This may include:
- A blood test to find out your cholesterol and blood sugar level
- checking your pulse for an irregular heartbeat
- taking a blood pressure measurement
Brain scans
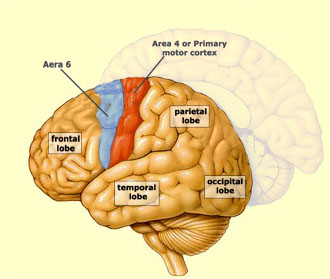
Even if the physical symptoms of a stroke are obvious, brain scans should also be done to determine:
- if the stroke has been caused by a blocked artery (ischaemic stroke) or burst blood vessel (haemorrhagic stroke)
- which part of the brain has been affected?
- how severe the stroke is?
Everyone with suspected stroke should have a brain scan within 1 hour of arriving at hospital.
An early brain scan is especially important for people who:
- might benefit from medicine to clear blood clots (thrombolysis), such as alteplase or early anticoagulant treatment
- are already taking anticoagulant treatments
- have a lower level of consciousness
This is why a stroke is a medical emergency and you should call 999 when a stroke is suspected – there’s no time to wait for a GP appointment.
The 2 main types of scans used to assess the brain in people who have had a suspected stroke are:
- CT scans
- MRI scan



CT scans
A CT scan is like an X-ray, but uses multiple images to build up a more detailed 3-dimensional picture of your brain to help your doctor identify any problem areas.
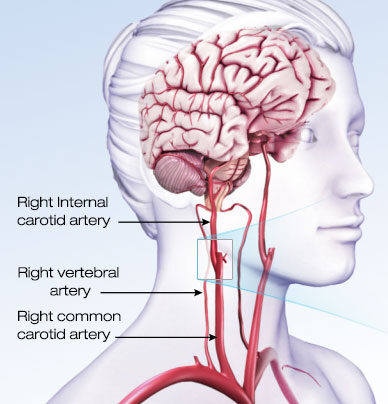
During the scan, you may be given an injection of a special dye into one of the veins in your arm to help improve the clarity of the CT image and look at the blood vessels that supply the brain.
If it’s suspected you’re experiencing a stroke, a CT scan is usually able to show whether you have had an ischaemic stroke or a haemorrhagic stroke.
It’s generally quicker than an MRI scan and can mean you’re able to receive appropriate treatment sooner.
MRI scans
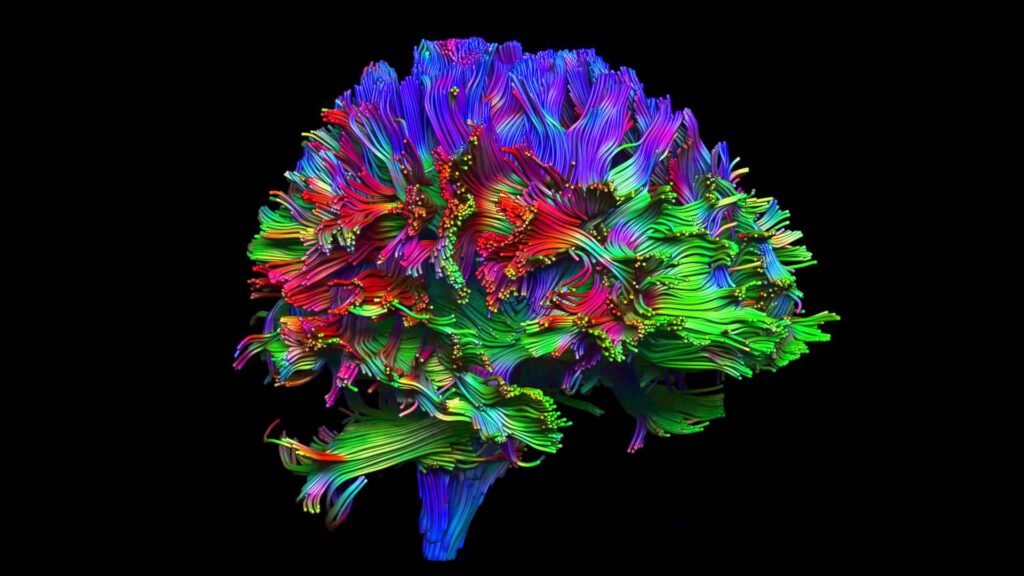
An MRI scan uses a strong magnetic field and radio waves to produce a detailed picture of the inside of your body.
It’s usually used in people with complex symptoms, where the extent or location of the damage is unknown.
It’s also used in people who have recovered from a transient ischaemic attack (TIA).
This type of scan shows brain tissue in greater detail, allowing smaller, or more unusually located, areas affected by a stroke to be identified.
As with a CT scan, special dye can be used to improve MRI scan images.
Treatment of ischemic stroke
Generally, there are three treatment stages for stroke: prevention, therapy immediately after the stroke, and post-stroke rehabilitation. Therapies to prevent a first or recurrent stroke are based on treating an individual’s underlying risk factors for stroke, such as hypertension, atrial fibrillation, and diabetes. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving or removing the blood clot causing an ischemic stroke or by stopping the bleeding of a hemorrhagic stroke.
The most popular classes of drugs used to prevent or treat stroke are antithrombotics (antiplatelet agents and anticoagulants) and drugs that break up or dissolve blood clots, called thrombolytics.
Emergency IV medication. Therapy with drugs that can break up a clot has to be given within 4.5 hours from when symptoms first started if given intravenously. The sooner these drugs are given, the better. Quick treatment not only improves your chances of survival but also may reduce complications.
An IV injection of recombinant tissue plasminogen activator (tPA) — also called alteplase (Activase) — is the gold standard treatment for ischemic stroke. An injection of tPA is usually given through a vein in the arm with the first three hours. Sometimes, tPA can be given up to 4.5 hours after stroke symptoms started.
This drug restores blood flow by dissolving the blood clot causing your stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine if tPA is appropriate for you.
Emergency endovascular procedures. Doctors sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to significantly improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible:
- Medications delivered directly to the brain.Doctors insert a long, thin tube (catheter) through an artery in your groin and thread it to your brain to deliver tPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected tPA, but is still limited.
- Removing the clot with a stent retriever.Doctors can use a device attached to a catheter to directly remove the clot from the blocked blood vessel in your brain. This procedure is particularly beneficial for people with large clots that can’t be completely dissolved with tPA. This procedure is often performed in combination with injected tPA

Prognosis
Recurrent stroke is frequent about 25 percent of people who recover from their first stroke will have another stroke within 5 years
Hemorrhagic stroke
Hemorrhagic stroke occurs when a blood vessel in your brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect your blood vessels. Factors related to hemorrhagic stroke include:
- Uncontrolled high blood pressure
- Overtreatment with blood thinners (anticoagulants)
- Bulges at weak spots in your blood vessel walls (aneurysms)
- Trauma (such as a car accident)
- Protein deposits in blood vessel walls that lead to weakness in the vessel wall (cerebral amyloid angiopathy)
- Ischemic stroke leading to hemorrhage
A less common cause of bleeding in the brain is the rupture of an abnormal tangle of thin-walled blood vessels (arteriovenous malformation).