HEADACHE
Headaches are a very common condition that most people will experience many times during their lives.
Headaches are a major cause of absenteeism from work and school. They also take a toll on social and family life. For some people, continually battling headaches can lead to feeling anxious and depressed.
Types Of Headache
There are more than 150 types of headache. They fall into two main categories: primary and secondary headaches.
Primary headaches
Primary headaches are those that aren’t due to another medical condition. The category includes:
- Cluster headaches.
- Migraine.
- New daily persistent headaches (NDPH).
- Tension headaches.
Secondary headaches
Secondary headaches are related to another medical condition, such as:
- Disease of blood vessels in the brain.
- Head injury.
- High blood pressure (hypertension).
- Infection.
- Medication overuse.
- Sinus congestion.
- Trauma.
- Tumor.
causes
- Headache pain results from signals interacting among the brain, blood vessels and surrounding nerves.
- During a headache, an unknown mechanism activates specific nerves that affect muscles and blood vessels. These nerves send pain signals to the brain.
- Researchers think migraines result when unstable nerve cells overreact to various factors (triggers). The nerve cells send out impulses to blood vessels and cause chemical changes in the brain. The result is disabling pain.
Symptoms
Headaches have a tendency to run in families, especially migraines. Children who have migraines usually have at least one parent who also suffers from them.
In fact, kids whose parents have migraines are up to four times more likely to develop them too.
Headaches can also be triggered by environmental factors shared in a family’s household, such as:
- Eating certain foods or ingredients, like caffeine, alcohol, fermented foods, chocolate and cheese.
- Exposure to allergens.
- Secondhand smoke.
- Strong odors from household chemicals or perfumes.
TRIGGERS
Common triggers of tension headaches or migraines include:
- Alcohol use.
- Changes in eating or sleeping patterns.
- Depression.
- Emotional stress related to family and friends, work or school.
- Excessive medication use.
- Eye, neck or back strain caused by poor posture.
- Lighting.
- Noise.
- Weather changes.
LOCATION
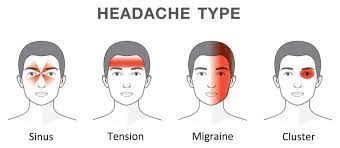
Migraines
Migraines are the second most common type of primary headaches. Symptoms of migraines include:
- Moderate to severe pain.
- Nausea or vomiting.
- Pounding or throbbing pain.
- Pain that lasts four hours to three days.
- Sensitivity to light, noise or odors.
- Stomach upset or abdominal pain.
Tension type headaches
Tension headaches are the most common type of headache. Tension headache pain tends to be:
- Consistent without throbbing.
- Mild to moderate.
- On both sides of the head (bilateral).
- Responsive to over-the-counter treatment.
- Worse during routine activities (such as bending over or walking upstairs).
Cluster headaches
Cluster headaches are the most severe type of primary headache.
They occur one to eight times per day during a cluster period, which may last two weeks to three months.
The headaches may disappear completely (go into remission) for months or years, only to recur later.
The pain of a cluster headache is:
- Intense with a burning or stabbing sensation.
- Located behind one of your eyes or in the eye region, without changing sides.
- Throbbing or constant.
New daily persistent headaches
This is one of the newest type of headache.
New daily persistent headaches (NDPH) come on suddenly and last for more than three months.
They typically occur in people who weren’t having frequent headaches before.
The pain of NDPH is:
- Constant and persistent without easing up.
- Located on both sides of the head.
- Not responsive to medications.
Sinus headaches
Sinus headaches are the result of a sinus infection, which causes congestion and inflammation in the sinuses (open passageways behind the cheeks and forehead).
People, and even healthcare providers, often mistake migraines for sinus headaches.
Symptoms of sinus headaches include:
- Bad taste in mouth.
- Deep, constant pain in your cheekbones and forehead.
- Facial swelling.
- Feeling of fullness in ears.
- Fever.
- Pain that gets worse with sudden head movement or straining.
- Mucus discharge (snot).
Medication overuse headaches
Medication overuse headaches (MOH) or rebound headaches affect up to 5% of people. They happen when you frequently take pain relievers for headaches.
This practice can actually increase your number of headaches. Signs of MOH include:
- Headaches becoming more frequent.
- More days with headaches than without.
- Pain that’s worse in the morning.
Headaches in children
Most kids have had a headache by the time they get to high school. For about 20% of them, tension headaches and migraines are a reoccurring problem.
Similar to adults, triggers for headaches in children include:
- Certain foods that trigger headaches for the individual.
- Changes in sleep.
- Environmental factors.
- Stress.
For you or your child has any of these headache symptoms, get medical care right away:
- A sudden, new, severe headache
- A headache that is associated with neurological symptoms such as:
- Weakness
- Dizziness
- Sudden loss of balance or falling
- Numbness or tingling
- Paralysis
- Speech difficulties
- Mental confusion
- Seizures
- Personality changes/inappropriate behavior, or
- Vision changes (blurry vision, double vision, or blind spots)
- Headache with a fever, shortness of breath, stiff neck, or rash
- Headache pain that awakens you up at night
- Headaches with severe nausea and vomiting
- Headaches that occur after a head injury or accident
- Getting a new type of headache after age 55
RED ALERTS Symptoms associated with headache.
It requires an appointment with your health care provider or a headache specialist
Contact your health care provider if you or your child has any of the following symptoms:
- Three or more headaches per week.
- Headaches that keep getting worse and won’t go away.
- Need to take a pain reliever every day or almost every day for your headaches.
- Need more than 2 to 3 doses of over-the-counter medications per week to relieve headache symptoms.
- Headaches that are triggered by exertion, coughing, bending, or strenuous activity.
ASSOCIATED SYMPTOMS WITH HEADACHE
- A history of headaches, but have noticed a recent change in your headache symptoms.
- Confusion or slurred speech.
- Fever.
- Headache after head injury.
- Severe headache that comes on suddenly or headache that doesn’t go away.
- Seizures or loss of consciousness.
- Multiple headaches in children.
- Stiff neck, or pain in the ear or eye.
- Weakness or numbness.
DURING OPD VISIT DO READY WITH ANSWER OF FOLLOWING QUESTIONS.
During the headache evaluation, your provider will ask you about your headache history, including:
- A description of your headaches.
- What the headaches feel like.
- How often the headaches happen.
- How long the headaches last each time.
- How much pain the headaches cause you.
- What foods, drinks or events trigger your headaches.
- How much caffeine you drink each day.
- What your stress level are.
- What your sleep habits are like.
- If you have any work issues.
Your headache can be more accurately diagnosed by knowing:
- When the headache started.
- How long you have had the headache.
- Whether there is a single type of headache or multiple types of headaches.
- How often the headache occurs.
- What causes the headache, if known (for example, do certain situations, foods, or medications usually trigger the headache?).
- If physical activity aggravates the headache pain.
- What events are associated with the headache.
- Who else in your family has headaches.
- What symptoms, if any, occur between headaches.
Your doctor will also ask additional questions about performance at work, family background, and if there is any history of drug abuse.
Clinical description of headaches
- Where the pain is located.
- What it feels like.
- How severe the headache pain is, using a scale from 1 (mild) to 10 (severe).
- If the headache appears suddenly without warning or with accompanying symptoms.
- What time of day the headache usually occurs.
- If there is an aura (changes in vision, blind spots, or bright lights) before the headache.
- What other symptoms or warning signs occur with the headache (weakness, nausea, sensitivity to light or noise, decreased appetite, changes in attitude or behavior).
History of headache treatments
MOST important in headache evaluation is medication history , which is usually missed .
You should provide your physician with a history of prior headache treatments.
Tell your doctor what medications you have taken in the past and what medications are you currently taking.
Don’t hesitate to list them, bring in the medication bottles or ask your pharmacist for a printout.
If any studies or tests were previously performed, bring them with you.
This may save time and repetition of tests.
SIGNS TO LOOK FOR COMPLAINTS OF HEADACHE
These signs and symptoms can include:
- Fever
- High blood pressure
- Muscle weakness, numbness, or tingling
- Excessive fatigue, wanting to sleep all of the time
- Loss of consciousness
- Balance problems, falling
- Vision problems (blurry vision, double vision, blind spots)
- Mental confusion or changes in personality, inappropriate behavior, speech difficulties
Neurological tests focus on ruling out diseases that might also cause headaches, such as epilepsy, multiple sclerosis, and other cerebrovascular diseases.
A disorder of the central nervous system might be suspected in the development of serious headaches. These include:
- Tumor
- Abscess
- Hemorrhage (bleeding within the brain)
- Bacterial or viral meningitis (an infection or inflammation of the membrane that covers the brain and spinal cord)
- Pseudotumor cerebri (increased intracranial pressure)
- Hydrocephalus (abnormal build-up of fluid in the brain)
- Infection of the brain
- Encephalitis (inflammation of the brain)
- Blood clots
- Head trauma
- Sinus blockage or disease
- Malformation (such as Arnold-Chiari)
- Injuries
- Infections, such as Lyme disease
- Meningitis
- Aneurysm
TREATMENT
Once you know your triggers, your neurologist can tailor treatment to you.
Counseling and stress management techniques can help you handle this trigger better.
Stress management
Stress management teaches you ways to cope with stressful situations.
Relaxation techniques – deep breathing, muscle relaxation, mental images and music to ease your tension.
Biofeedback
Biofeedback teaches you to recognize when tension is building in your body. You learn how your body responds to stressful situations and ways to settle it down.
Medications
Occasional tension headaches usually respond well to over-the-counter pain relievers. But be aware that using these medications too often can lead to a long-term daily headache.
Drugs for high blood pressure, seizures and depression can sometimes prevent migraines. Your neurologist provider may recommend trying one of these medications to reduce headache frequency.
self-care treatments for headaches include:
- Applying heat or cold packs to your head.
- Doing stretching exercises.
- Massaging your head, neck or back.
- Resting in a dark and quiet room.
- Taking a walk.